American Heart Association (AHA) Updates Guidance for CPR - How Nurses Feel
In October 2021, the American Heart Association (AHA) updated its guidelines for healthcare professionals performing CPR on patients who have confirmed infection with COVID. Their message? Don’t delay cardio-pulmonary resuscitation (CPR) to put on a mask.
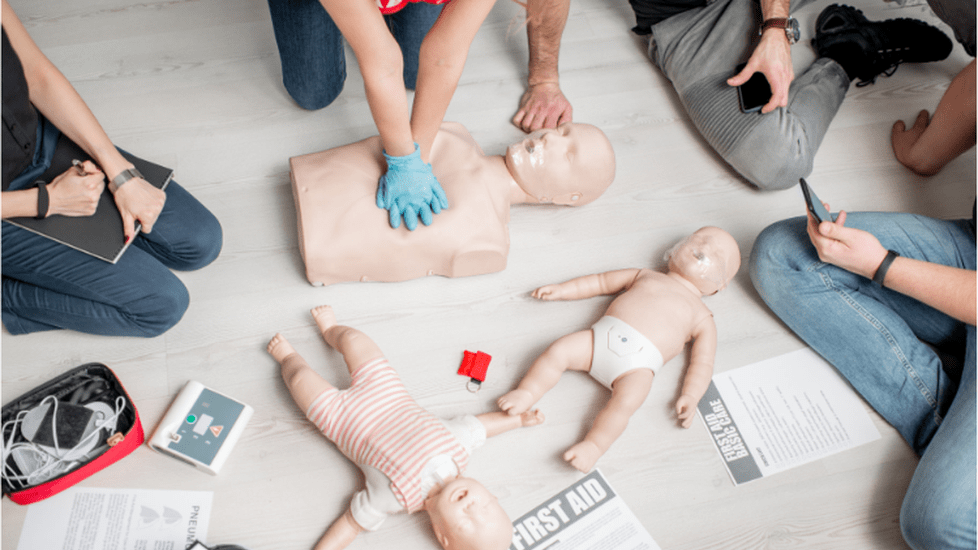
The updated guidelines apply to all patient populations, from adults (including pregnant adults) to pediatric and neonates with known or suspected COVID, and are based after early-pandemic data found poor cardiac outcomes that can be attributed in part to delays in care with cardiac arrests. Here’s what healthcare professionals need to know about the changes.
How the Guidelines Shifted
The update to the guidelines is a significant one because they haven’t been updated since April 2020—which, as you may recall, was a very difficult and dangerous time during the pandemic. The AHA guidelines encouraged personal protection equipment (PPE) and early intubation and airway control to minimize the spread of the virus whenever performing CPR.
And without specific knowledge of the virus’s transmission and a significant lack of PPE for healthcare workers, chest compressions were being delayed during that time period out of precautions, which did result in more poor outcomes for those suffering cardiac events both in and out of the hospital at the beginning of the pandemic. The AHA also noted that people may have delayed care as well, which could have contributed to the increase in negative outcomes.
With these factors in mind—and more knowledge about the virus, along with increased PPE access and vaccination among most healthcare workers-–the AHA explained that “application of the best resuscitation science available must be once again assessed and prioritized.”
What the New Guidelines Say
In general, the guidelines send this important message: don’t delay CPR to put on PPE. That applies to both you and the patient, so don’t try to put on a mask for either you or the patient if one is not readily available. Essentially, if you come across someone in need of resuscitation who is known or suspected to have COVID-19, you should start chest compressions immediately and call for backup of providers who have time to don PPE and can relieve you.
The AHA stressed that timely medical attention is given to those in need of CPR. The AHA pointed out that while PPE and appropriate precautions should always be used, the risk of a COVID-19-infected patient with a cardiac arrest dying as a result of delayed care (to don PPE) is much higher than the risk a healthcare provider will get the virus from them and develop a serious illness, especially if the provider is vaccinated and appropriate PPE is worn.
CPR Guidelines for Known/Suspected COVID Patients
In general, the recommendations for delivering CPR to a suspected or known COVID-19 infected person are:
- Step 1. As a healthcare provider, ensure that you are vaccinated and/or boosted as appropriate to best protect yourself against infection.
- Step 2. Begin chest compressions immediately. Do not delay or stop compressions to put on PPE. Defibrillation should be initiated ASAP as needed, also without delaying for PPE.
- Step 3. Additional providers should be called as soon as possible and put on PPE before relieving the initial resuscitator.
- Step 4. When providers in PPE arrive - step out to don your own PPE and then continue providing care.
Other Recommendations
The new AHA guidelines for CPR for COVID-infected or suspected patients also include specific recommendations for airway and circulation in different patient populations, as well as general recommendations for providing care, such as:
- Keep healthcare providers safe by using appropriate PPE. Appropriate PPE includes N-95 respirators, eye protection, bag-make ventilation, intubation, and positive pressure ventilation, as appropriate.
- Communicate the patient’s COVID-19 status and ensure any new providers have adequate PPE.
- Consider passive oxygenation until a HEPA-filtered device for agonal breathing. May consider using a surgical facemask overlaid until the HEPA-filtered device can be applied.
- Use HEPA filters with any ventilation device.
- Ensure a tight seal when using a 2-person technique for bag-mask-HEPA-filter device set-up.
- Newborn babies are very unlikely to spread COVID-19.
- There are also specific guidelines for ventilator settings and techniques.
How Nurses Feel About the Guidelines
So what do healthcare providers actually think of the new guidelines?
The updated guidelines, in combination with the CDC’s announcement of shortened isolation timelines for asymptomatic COVID-infected nurses to return back to work, have led some healthcare providers to feel that their own health is not being prioritized.
“Treating health care workers like they are expendable and gambling with their lives in this way is just unacceptable,” wrote Kaela on Facebook. “Please, keep yourselves safe while caring for others,” she added in a plea to her fellow providers. “It’s like when you’re on an airplane— you have to put on your own oxygen mask first before helping others. Stay safe out there!”
Commenters on MedPage Today’s article about the update were also less than impressed.
“So now we have enough healthcare professionals that we can sacrifice them to do CPR on a patient with a probable poor outcome whether or not we start CPR in 30 seconds or 1 minute?” wrote Maureen. “Putting on my N95 takes 15 seconds. My eyewear is always on top of my head and easy to flip down. Is this article talking about in-hospital arrest or out-of-hospital arrest? I am even more disheartened about the idea that we are all sacrificial lambs to the slaughter. I would like the persons at the AHA to follow me on a shift in the Covid ICU and respond to codes and start CPR without PPE. Do they practice what they suggest?”
Carolannexpressed a similar statement on the American Academy of Critical Care Nurses (AACN)’s blog, writing, “Are you kidding me? We are to risk getting COVID doing CPR without PPE? I don't think so.”
And Darylene Hoover posted a frustrated statement on Facebook, writing, “Why are we reverting back to not protecting ourselves first? Also, have any of the people making these guidelines actually done CPR on someone? It’s not uncommon for all kinds of secretions to come out of the patient’s mouth. You’re telling me that none of this is being aerosolized potentially? …. We have officially thrown infection control out the window,” she concluded.
Meanwhile, Laurie O'Daniel Piestrup also pointed out on Facebook that it’s not just COVID-19 that healthcare providers could be exposed to with CPR, so the guidelines may be overlooking that important fact.
“They had cooties before C19,” she quipped.
What do you think? Do the new CPR guidelines make sense or will you be donning a mask before performing CPR on a patient?





